Getting sick is inevitable.
For most, when that happens, they go to their doctor, and their insurance covers the majority of the cost of the visit. But what happens if their insurance doesn’t cover the cost at all?
That is the new reality for Cardajah Burns, freshman in political science. This past September, she got sick and had chest pains, so she went for a routine checkup at the Auburn University Medical Clinic.
Burns receives insurance coverage through Medicaid. In her hometown of Chelsea, it was generally accepted. At the Auburn University Medical Clinic, however, she quickly discovered otherwise.
When Burns arrived at the AUMC, she was filling out information at a kiosk that asked whether or not she had insurance. When she indicated no, the kiosk prompted her to talk to the front desk.
“They were like, ‘Yeah, we don’t accept Medicaid, sorry,’” Burns said. “Then I had to pay for it.”
She said they informed her that the AUMC did not accept Medicaid and offered her no real explanation why. Burns said she had no other choice but to pay the fees, and when she told the front desk, they seemed surprised.
“She said, ‘I’m assuming you’re really sick considering you still want to see us,’” Burns recalls the worker at the front desk telling her.

According to the AUMC website, the clinic is not an approved Medicare or Medicaid provider. Students with those coverage plans are responsible for the payment of their visit.
To be able to accept Medicaid as a form of insurance, a medical clinic or other healthcare provider must enroll in their respective state’s Medicaid program. Each state’s Medicaid program decides what people and services will be covered, according to the Alabama Medicaid Agency.
The type of coverage is usually dependent on how much the state can afford. The federal government will provide matching funds as long as the federal minimum requirements are met.
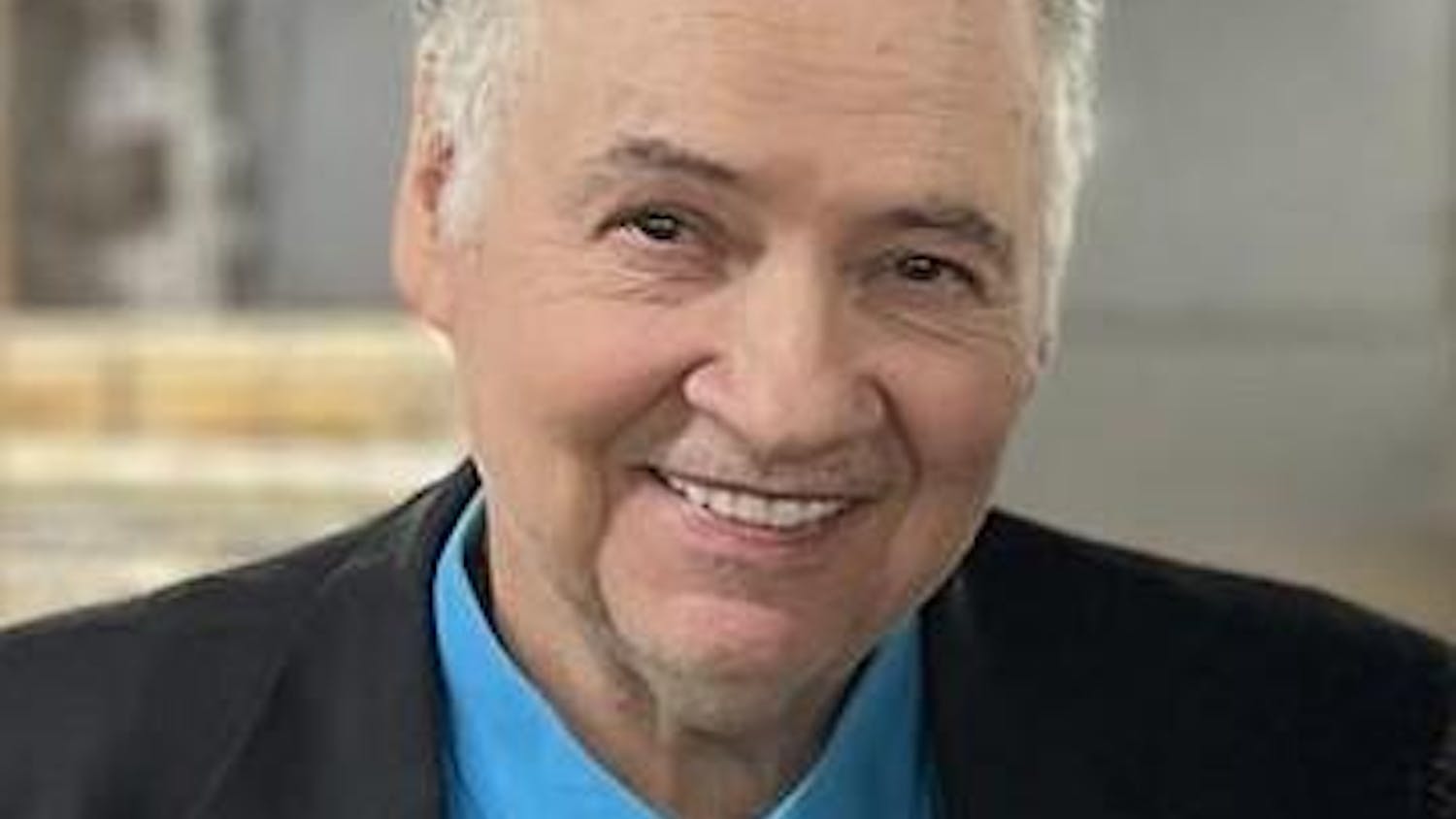
Fred Kam, director of the AUMC, said the decision was a financial one.
“[The reason] is really simple: at the end of the day, it’s a business decision,” Kam said. “The reimbursement from Medicaid for services in the visit tends to be below our cost of doing business.”
When a medical clinic or any other type of health provider gives care to an individual with insurance, that individual’s insurance is billed for the cost of the care that was given. In most cases, an individual’s insurance reimburses the health provider for the large majority of the cost of the care, if not the entire cost.
“Let’s say someone needed a tetanus shot. It costs us, for argument’s sake, $40 to purchase the vaccine. Then on top of that, we have to have a nurse to give it, you have to use a syringe and needle, an alcohol pad … whatever,” Kam said. “At the end of the day, to administer that vaccine, it might cost us $50 dollars.”
However, according to Kam, Medicaid gives by far the worst reimbursement for services rendered by the med clinic, a reimbursement rate similar to that of Tricare Prime, a military-based insurance.
Kam gave a hypothetical example of the reimbursement rate of Tricare Prime to illustrate the large gulf between costs and reimbursement with Medicaid.
“Tricare Prime says, ‘We’ll pay you $20,’” Kam said. “So we lose $30 dollars to do what we medically believe is right to do, and that’s [giving] that tetanus shot, but now we’re being paid $20 dollars for what’s costing us $50.”
If the AUMC accepted Medicaid as a form of insurance, every time they saw a patient and provided care, they would be losing money, according to Kam. The AUMC would have to subsidize its care.

Kam said some of the regulatory requirements that come with Medicaid make signing up for it even less enticing.
“If we signed up as a Medicaid provider, then we would have to open our potential services to any and all Medicaid recipients, and they don’t have to be Auburn University-related,” Kam said. “That’s not something we want to do, either.”
Unfortunately for those on Medicaid at Auburn, Kam said this stance seems to be shared by many different healthcare providers in the area.
“If you call just about any doctor’s practice, except pediatricians, here in Auburn or Opelika, you will find that pretty much almost none provide care for Medicaid,” Kam said. “The only offices I think you will see that will provide care for Medicaid are pediatrician offices and OBGYN offices.”
The reason these practices are willing to provide care for those with Medicaid is due to the increased reimbursement rate. The rate of coverage that Medicaid provides for kids and pregnant women is higher than for young adults, according to Kam.
This difference in the reimbursement rate may be due to the demographics that Medicaid covers. According to the Alabama Medicaid Agency, Medicaid is a state-run program funded by both state and federal government that pays for medical and long-term care services for low-income pregnant women, children, certain people on Medicare, disabled individuals and nursing home residents.
The agency also outlines the eligibility of college students, saying that students can be on Medicaid if they are under 19, if they are a foster child under the age of 26, a low-income parent, a pregnant woman or a number of more specific cases.
Kam said the majority of Auburn students on Medicaid will fall into the under-19 category, and because the proportion of Auburn students who fall into this category is relatively small, the benefits are not enough to outweigh the costs.

“We’re trying to do the best that we can for the majority that we can,” Kam said. “It is impossible for us to be everything to everyone, and we’ve got to make business decisions that help us serve the vast majority and maintain the quality of the care that we deliver on a consistent basis.”
To Kam, all of that makes good business sense, but it doesn’t help students like Burns. When she went to the AUMC to seek care, the chest pain she came with was a recurring condition called pleurisy, an inflammation of the tissues that line the lungs.
Pleurisy is easily treatable, but if Burns comes down with it again, she will have to either pay the fees out of pocket or find somewhere else to go. It’s inconvenient, she said.
For medical visits, sometimes the cost of the checkup can be much more expensive than the actual medicine or treatment needed.
Students with accepted forms of insurance rarely notice this disparity, as insurance often covers it. For those without it, however, this price can be daunting. This is true even while keeping in mind that students paying out of pocket are given a discount.
“The visit was $81, and the medicine I had to buy was like $15,” Burns said.
Her visit was for a routine illness. One could expect a more serious illness or injury to cost even more.
For Burns, the only thing she wants now is to forget about her whole situation.
“At the time, I was a little upset about it. I’m not really upset about it now,” Burns said. “I just try not to worry about it. If I’m sick enough, I’ll find somewhere else to go, I guess.”
Do you like this story? The Plainsman doesn't accept money from tuition or student fees, and we don't charge a subscription fee. But you can donate to support The Plainsman.