A University professor has received a grant to continue his research in medication management for people with mental health issues.
Richard Hansen, department head in health outcomes research and policy in the Harrison School of Pharmacy, is the recipient of a grant subaward from the Agency for Healthcare Research and Quality to continue his research in medication management for people with mental health issues.
The first grant, which expired in 2012, focused on veterans and whether having a bad healthcare experience is because they had chronic conditions or because they saw several doctors.
"In our prior work, we found that for patients with multiple conditions and taking multiple medications, the most important predictor of having poor treatment outcomes was how many different providers were involved in the patients' care," Hansen said.
Hansen said confusion is created when patients see multiple doctors at the same time.
"So, you get one doctor prescribing one thing and another doctor prescribing another and no one is talking to each other, which creates a big old mess," Hansen said.
Hansen said the biggest surprise to him in the first study was how adding one doctor to a handful of others increases the risk of making an emergency room visit.
"We thought that the number of doctors would be an important point, but we were surprised by the fact that each doctor you add on, you increase that risk by about 50 percent," Hansen said.
The second study, which adds mental health issues, will allow Hansen and his team of researchers to test the impact of having a medical care coordinator for patients with multiple illnesses.
Hansen said this should improve patients and doctors ability to balance all the illnesses.
"This study will allow us to further explore this phenomenon, specifically in a mental health population and test the impact of a medical home-care coordination model on outcomes," Hansen said. "This work can help guide the re-design of healthcare for better care coordination and better outcomes."
Hansen's work suggests there is evidence some healthcare providers poorly manage the existence of simultaneous but independent medical conditions in patients with schizophrenia.
One reason for the mismanagement is poor care coordination between psychiatric specialists treating the mental health needs of patients and primary care providers managing other symptoms.
The lack of coordination can result in inappropriate prescribing, duplication of medication therapy, medication non-adherence and more aggressive health service utilization for high expenditure intensive resources, according to Hansen.
"In some previous work that we did, we found that one of the biggest challenges with psychiatry and in particular with patients with schizophrenia is that they often get their primary point of care from psychiatrists, but psychiatrists are usually not comfortable managing the other chronic healthcare condition," Hansen said.
Hansen said this is especially difficult for people with multiple conditions.
"So, let's say that you have schizophrenia, but you also have diabetes and congestive heart failure," Hansen said. "The psychiatrist, in many cases, won't manage the other conditions. The primary care doctors or the other specialist won't manage the psychiatric aspect."
Hansen said the study results will improve the understanding of medication care coordination, the role of mental health in care coordination, and the benefits of the medical home model at improving care for patients with multiple chronic conditions.
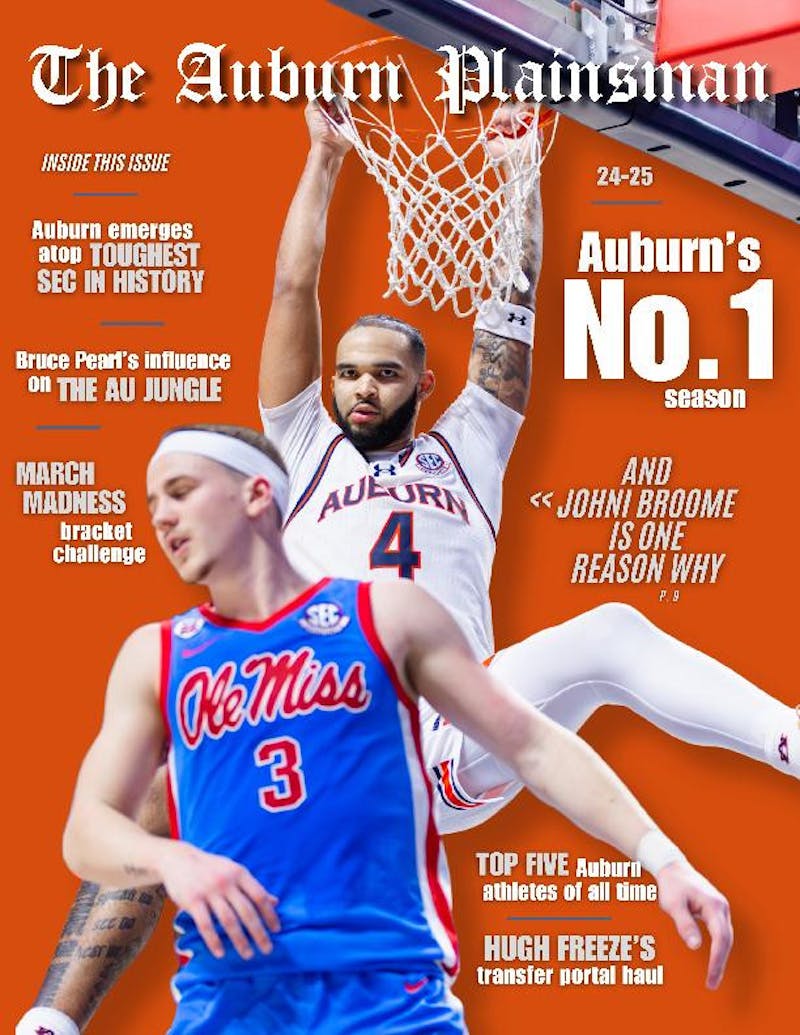
Do you like this story? The Plainsman doesn't accept money from tuition or student fees, and we don't charge a subscription fee. But you can donate to support The Plainsman.